Breakthrough Personalized Vaccine Shows Promise in Fighting Deadly Pancreatic Cancer

Pancreatic ductal adenocarcinoma (PDAC), the most common and deadliest form of pancreatic cancer, continues to pose a significant challenge in terms of effective treatment. Despite advancements in therapies, the survival rate for individuals diagnosed with PDAC remains alarmingly low, with only about 12% surviving beyond five years of treatment.
In a groundbreaking development, a research team led by Dr. Vinod Balachandran from Memorial Sloan Kettering Cancer Center (MSKCC), funded by the National Institutes of Health (NIH), has made significant progress in harnessing immunotherapies to combat PDAC. Immunotherapies, which bolster the body’s immune system to attack tumors, have transformed the treatment landscape for many cancer types. However, their effectiveness in PDAC has been limited thus far, largely due to the uncertainty surrounding the production of neoantigens—proteins that can be targeted effectively by the immune system—by pancreatic cancer cells.
Building on this challenge, Dr. Balachandran’s team has developed a personalized mRNA cancer-treatment vaccine approach, aimed at enabling immune cells to recognize specific neoantigens present in patients’ pancreatic cancer cells. The results of a small clinical trial for this experimental treatment were published on May 10, 2023, in the esteemed journal Nature.
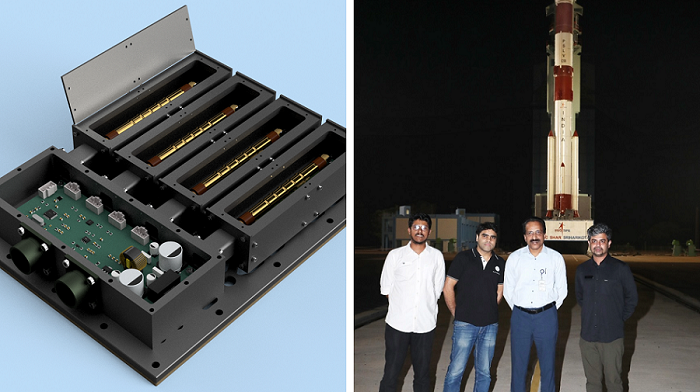
Following surgical removal of PDAC, the team collaborated with BioNTech, the company responsible for producing one of the mRNA COVID-19 vaccines, to analyze tumor samples from 19 patients. BioNTech conducted gene sequencing on these samples to identify proteins that could potentially trigger an immune response. This information was then utilized to create a personalized mRNA vaccine tailored to each patient, with each vaccine targeting up to 20 neoantigens.
Remarkably, customized vaccines were successfully developed for 18 out of the 19 study participants, with the entire process—from surgery to the administration of the first vaccine dose—taking an average of approximately nine weeks.
Prior to vaccination, all patients received a drug called atezolizumab, an immune checkpoint inhibitor that prevents cancer cells from suppressing the immune system. The personalized vaccines were subsequently administered in nine doses over several months. After the first eight doses, participants also commenced standard chemotherapy drugs for PDAC, followed by a ninth booster dose.
Among the 16 patients who remained healthy enough to receive some of the vaccine doses, half experienced activation of powerful immune cells known as T cells, which exhibited recognition capabilities specific to the patient’s pancreatic cancer. To monitor the T cells generated post-vaccination, the research team collaborated with the laboratory of Dr. Benjamin Greenbaum at MSKCC to develop a novel computational strategy. Through their analysis, the team discovered that T cells recognizing the neoantigens were absent in the blood prior to vaccination. Additionally, among the eight patients with robust immune responses, half exhibited T cells targeting more than one vaccine neoantigen.
Remarkably, at the year-and-a-half mark post-treatment, none of the individuals who exhibited a strong T cell response to the vaccine experienced cancer recurrence. In contrast, those patients whose immune systems did not respond favorably to the vaccine faced a cancer recurrence within just over a year, on average. Notably, one patient with a robust response witnessed the T cells generated by the vaccine successfully eliminating a small tumor that had metastasized to the liver. These compelling results indicate that the T cells activated by the personalized vaccines effectively suppressed the growth of pancreatic cancers.